In order to manage a patient suferring from sepsis, you must first know the stage of sepsis the patient is suffering from because the management is different for each stage.
Sepsis is defined as systemic inflammatory response syndrome as a result of an infectious process.
There are four stages of sepsis
- SIRS (Systemic Inflammatory Response Syndrome)
- Sepsis
- Severe Sepsis
- Septic Shock
Stage 1. SIRS
SIRS is an abbreviation of systemic inflammatory response syndrome,
It is defined as a response of the body from a non-specific insult. If a patient has two of the following features present, then we will label him as a case of SIRS.
- Temperature greater than 38 (100.4 F) or less than 96.8 (96.8 F)
- Heart Rate greater than 90 beats per minute
- Respiratory rate greater than 20 per minute
- WBC greater than 12000/mm3 or less than 4000/mm3 or greater than 10% bands.
Stage 2. Sepsis
If a patient has SIRS as evident by having two out of four features of SIRS with evidence of an infectious process then we will label the patient as a case of sepsis secondary to some infection.
Stage 3: Severe Sepsis
Sepsis that is the systemic response to an infection associated with organ dysfunction, hypoperfusion or hypotension. For example if a patient has pneumonia and found to have WBC of 16000 and has a heart rate of 90 beats per minute associated with fever and found to have a BP of 90/60 and labs show a creatinine of 2.0 and urea of 200 then it means organ dysfunction has started also patient has hypotension, then such patient fits into the criteria of severe sepsis
Stage 4: Septic Shock
If a patient has severe sepsis (mention above), and his hypotension is unresponsive to initial fluid resuscitation and he shows evidence of organ dysfunction then it means he is in septic shock now.
So septic shock means sepsis-induced hypotension despite adequate fluid resuscitation along with the presence of organ dysfunction.
First, evaluate the patient if he fits into the criteria of SIRS;
Are any two of the following SIRS criteria are present and new to your patient?
- Temperature > 38.3 or < 36 degree Celsius
- Heart rate greater than 90 beats per minute
- WBC < 4000 or greater 12000/mm3 or > 10% immature cells are present.
- Respiratory rate greater than 20 breaths per minute
- Altered mental status
If a patient has any 2 features then it means he has SIRS.
Next step is to look for an evidence of infection.
Take history and find out if he is having any symptom pertinent to infection such as cough, sputum, chest pain, dysuria, abdominal pain, diarrhea, headache with neck stiffness, cellulitis, endocarditis.
Examine the patient for signs of infection such as fever, tachypnea, tachycardia, shortness of breath, coarse crepitation in the chest, abdominal tenderness, neck stiffness etc.
Check the labs, imaging and cultures.
If any stigmata of infection is found along with SIRS it means the patient is suffering from sepsis.
Once sepsis is confirmed next step is look into labs and check If the organs are working perfectly or their function has been compromised?
Check blood pressure, Check liver function test (AST, ALT, Alk Phos, Bilirubin) renal function test (Urea, BUN Creatinine) etc, Lactate level, INR and aPTT, if they all are normal it means patient has sepsis but not severe sepsis, if there is hypotension or deranged renal or liver function or
- Lactate > 4 mmol/L
- Urine output 0.5 ml/kg/hr for 2 hrs
- INR > 1.5
- aPTT > 60s
- Bilirubin 34micro mol/l
- O2 needed to keep SpO2 > 90%.
Then it means patient has “Severe Sepsis”
If hypotension is found, give a fluid challenge, if BP improves, then the patient has severe sepsis, but if BP doesn’t improve despite initial fluid challenge it means the patient has gone into septic shock.
The sepsis Six Pathway
- Give high flow oxygen via non-rebreather mask (Read also: Oxygen Administration Methods)
- Take blood cultures, and consider source control.
- Give empirical IV antibiotics within the first hour of presentation according to the local protocol.
- Start IV fluid resuscitation, Hartmann’s or equivalent
- Check Lactate Level
- Monitor hourly urine output consider catheterization within one hour.
Time is important.
Steps to be completed within 3 hours of time of presentation
- Measure lactate level
- Obtain blood cultures prior to administration of antibiotics.
- Administer broad-spectrum antibiotics
- Administer 30ml/kg crystalloid for hypotension or lactate > or equal to 4 mmol/L
These above 4 steps should be completed within 3 hours of presentation.
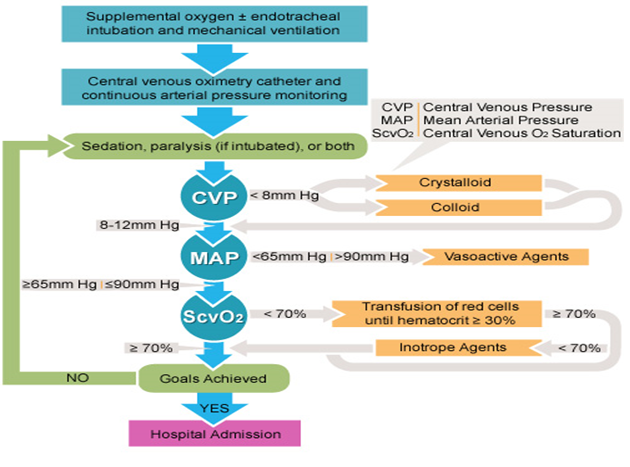
Steps to be completed within 6 hours of the time of presentation.
- Apply vasopressors, if hypotension doesn’t respond to initial fluid resuscitation to maintain mean arterial pressure (MAP) greater than or equal to 65mm Hg.
- IF there is persistent hypotension then measure
- Central venous pressure
- Aim is to keep CVP equal to or greater than 8 mmHg (8-12 mm Hg)
- Measure central venous oxygen saturation.
- Aim is to keep Central venous oxygen saturation (SCVO2) of 70% or more.
- If SCVO2 is less than 70% despite of oxygen therapy, or respiratory support then transfuse red cells unit until hematocrit reaches 30% or more.
- Re-measure lactate if initial lactate was elevated.
- Central venous pressure
After completing initial resuscitation (Sepsis Six)and diagnosis;
- Control the source of infection, check all the IV lines, cultures, and adjust the antibiotic therapy according to the sensitivity, drain if there is any abscess, debride the infective wound if necessary, surgical intervention for gangrenous, necrotizing viscera.
- Continue the fluid management without or without vasopressors (norepinephrine is vasopressor of choice, If there is cardiac dysfunction add dobutamine) and monitor vital signs and organ function, monitor labs, and urine output, goal is to keep mean arterial pressure greater than 65 mm Hg and keep urine output greater than 0.5ml/kg/hr.
- Add vasopressin (0.3 units per minute) if it is difficult to achieve MAP of 65 with vasopressors.
- If hypotension is not responding well to vasopressors and vasopressin combination therapy then there is a possibility that patient has adrenal insufficiency due to hypoperfusion, check serum cortisol levels and consider corticosteroid administration. Give 200mg of hydrocortisone daily.
- If Central venous oxygen saturation is less than 70% then transfuse blood products until Hem
 atocrit is more than 30%.
atocrit is more than 30%. - Monitor blood glucose level.
- Bicarbonate therapy to keep blood pH within normal range.
- The Antimicrobial regimen should be reassessed daily potential deescalation.
Other measures:
- Mechanical ventilation of Sepsis-induced ARDS (Acute respiratory distress syndrome)
- Glucose control. Monitor blood glucose 1-2 hourly until glucose values and insulin infusion rates are stable and then every 4 hours. Target upper glucose level is 180mg/dl.
- Continuous renal replacement therapies and intermittent hemodialysis are equivalent in patient with severe sepsis and acute renal failure.
- Use bicarbonate only if pH is less than 7.15.
- Deep venous thrombosis prophylaxis with low molecular weight heparin if there is no contraindication, may also use the intermittent pneumatic compression devices.
- Stress ulcer prophylaxis with pantoprazole preferably, or with H2 receptor blocker who have bleeding risk factors.
- Administer oral of enteral feedings as tolerated, rather than complete fasting or administration of IV glucose during the first 48 hours after the diagnosis of sepsis. Start with 500 calories per day and increase as tolerated.
- Procalcitonin level helps us to decide about discontinuation of antibiotics therapy. Discontinuation of antibiotics is strongly encouraged if Procalcitonin is less than 0.25.
- Good nursing care to avoid decubitus ulcers.
Special Thanks to
Dr. Sarah Azam Shah
Internal Medicine Resident, Pakistan Institute of Medical Sciences, Shaheed Zulfiqar Ali Bhutto Medical University PIMS Islamabad Pakistan.
Written by:
Dr. Adil Ramzan,
Internal Medicine Resident, Pakistan Institute of Medical Sciences, Shaheed Zulfiqar Ali Bhuto Medical University.